- Adapted from Murillo Perez CF, Harms MH, Lindor KD, et al. Am J Gastroenterol. 2020;115(7):1066-1074.
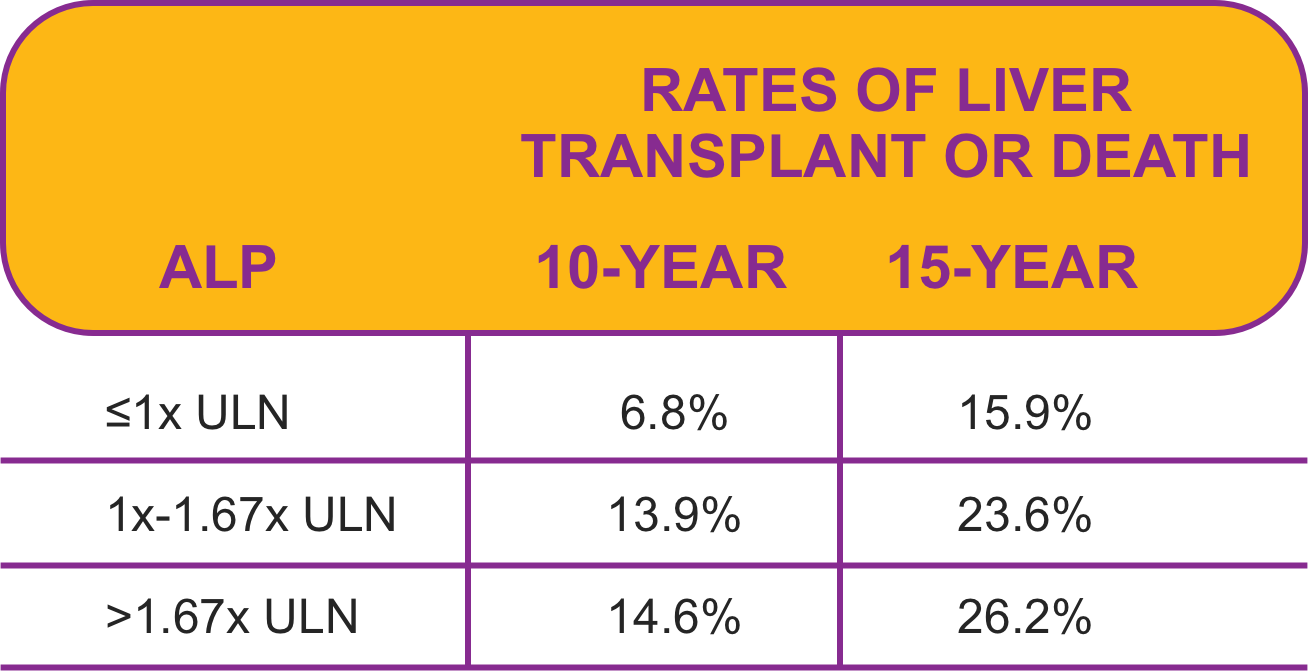
Survival Outcomes
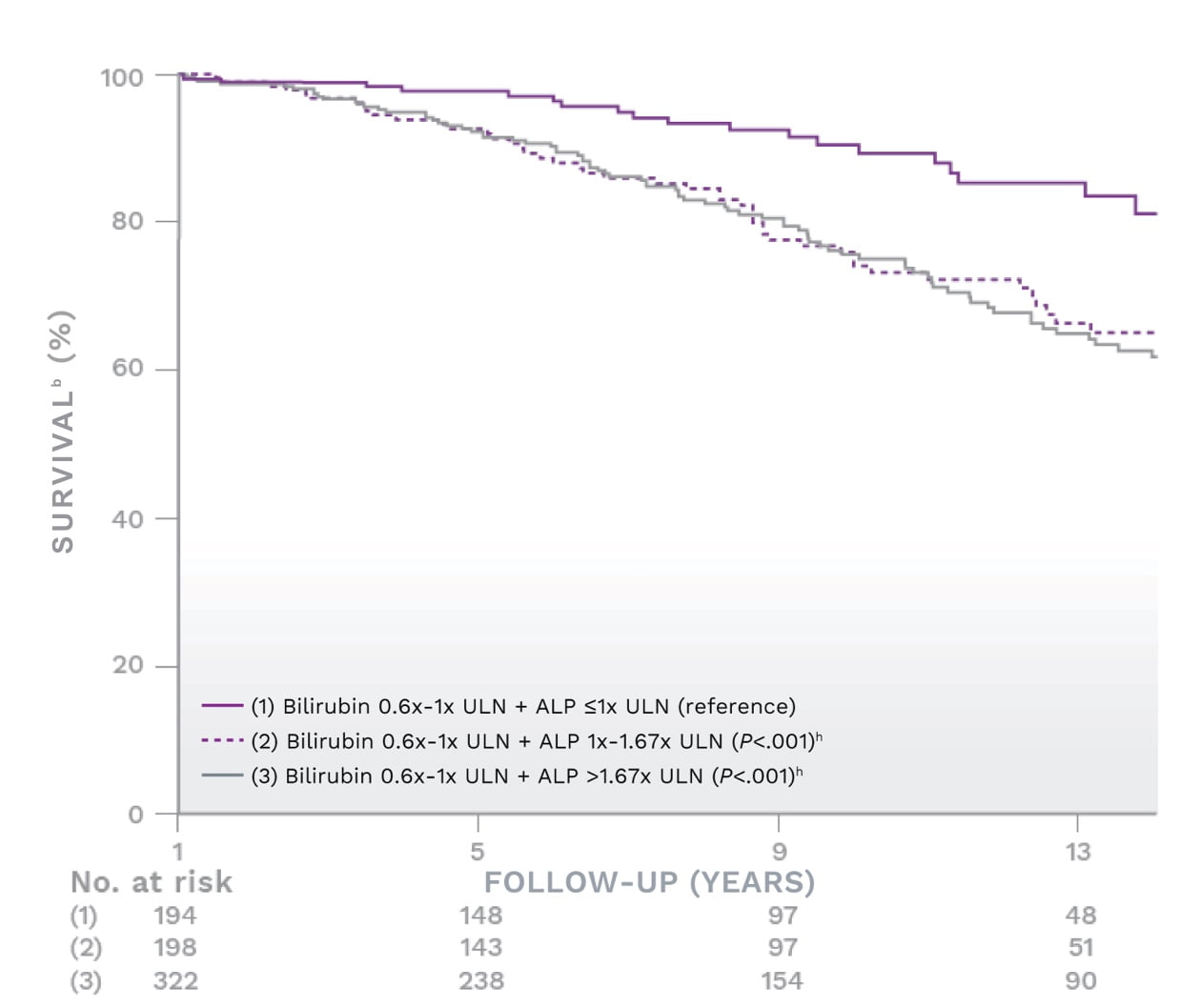
Based on the Global PBC Study Group, ALP levels between 1x-1.67x ULN had a similar risk of liver transplant or death as patients with levels up to 3x ULN1,2,a
≤1x ULN was the optimal threshold for ALP in a subgroup analysis of UDCA-treated patients with ALP ≤1.67x ULN and normal bilirubin at 1 year
Survival rate estimates
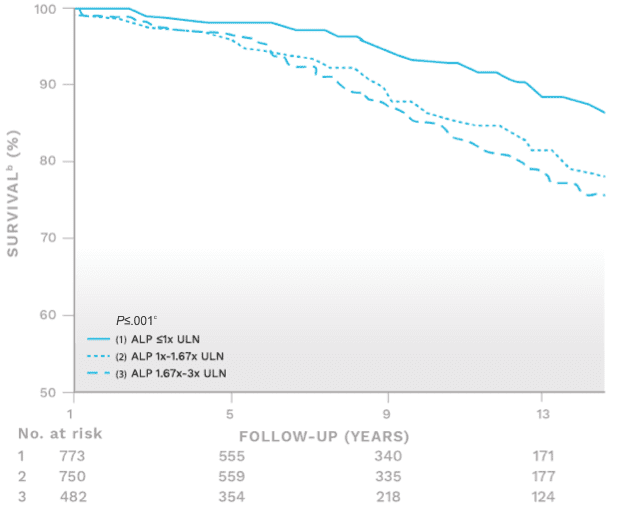
When ALP was >1x ULN,
the risk of liver transplant or death was 44% greater
than if ALP was ≤1x ULN (P=.03)
- Adapted from Murillo Perez CF, Harms MH, Lindor KD, et al. Am J Gastroenterol. 2020;115(7):1066-1074.
Bilirubin that surpasses 0.6x ULN was found to significantly increase risk1,2,d
The optimal threshold for bilirubin was found to be ≤0.6x ULN in this analysis of the Global PBC Study Group
Survival rate estimates
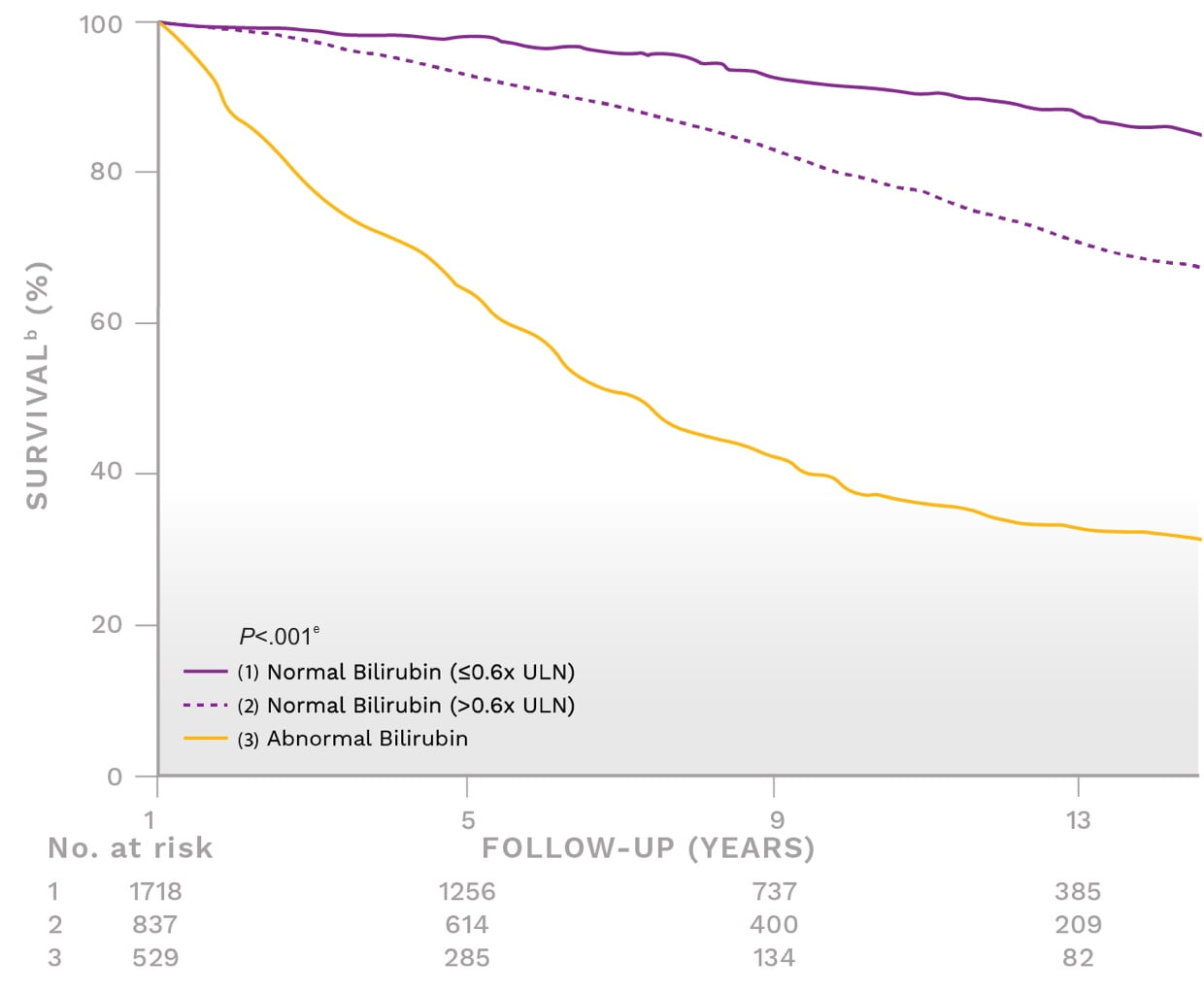
- Adapted from Murillo Perez CF, Harms MH, Lindor KD, et al. Am J Gastroenterol. 2020;115(7):1066-1074.
When bilirubin was >0.6x ULN,
>2x more patientsf had a liver transplant or died within 10 years
than if bilirubin was ≤0.6x ULN
- Adapted from Murillo Perez CF, Harms MH, Lindor KD, et al. Am J Gastroenterol. 2020;115(7):1066-1074.
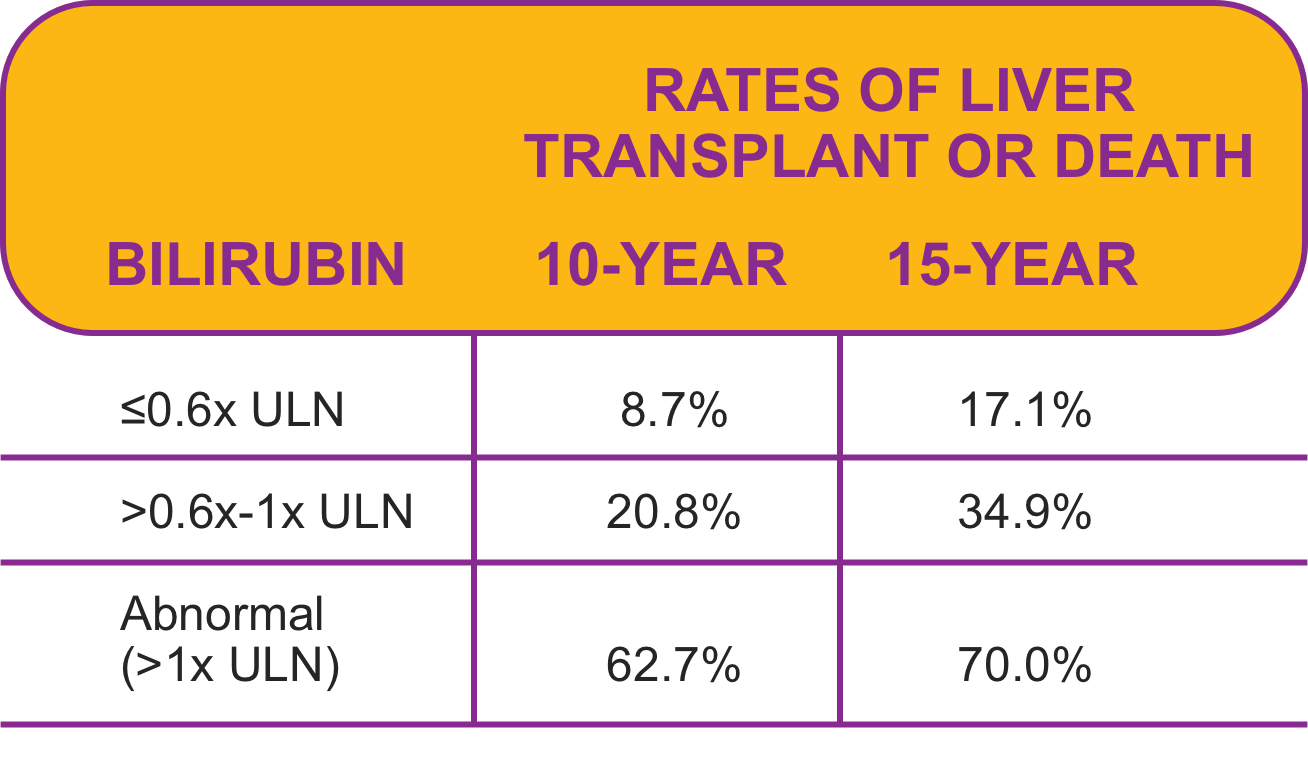
Normalizing ALP can offset the risk in patients with bilirubin 0.6x-1x ULN1,2,d
In a subset of patients with bilirubin levels of 0.6x-1x ULNg, a significant survival benefit was observed when ALP was normalized (ie, ≤1x ULN) compared to ALP 1x-1.67x ULN
Survival rate estimatesg
- Adapted from Murillo Perez CF, Harms MH, Lindor KD, et al. Am J Gastroenterol. 2020;115(7):1066-1074.
In patients with bilirubin 0.6x-1x ULNg,
the rate of liver transplant or death over 10 years increased 2.5xf
when ALP was above normal (>1.67x ULN) vs below (≤1x ULN) (~25% vs ~10%, respectively)
- Adapted from Murillo Perez CF, Harms MH, Lindor KD, et al. Am J Gastroenterol. 2020;115(7):1066-1074.
Fibrosis stage, as well as biomarkers, should be considered in PBC risk stratification3,i
Fibrosis stage categorized as early (stage 1/2) vs advanced (stage 3/4) was an independent predictor of transplant-free survival, despite biochemical response in another Global PBC Study Group analysis
- Patients with an advanced fibrosis stage had worse transplant-free survival rates despite treatment response j
Transplant-free survival rate estimatesk
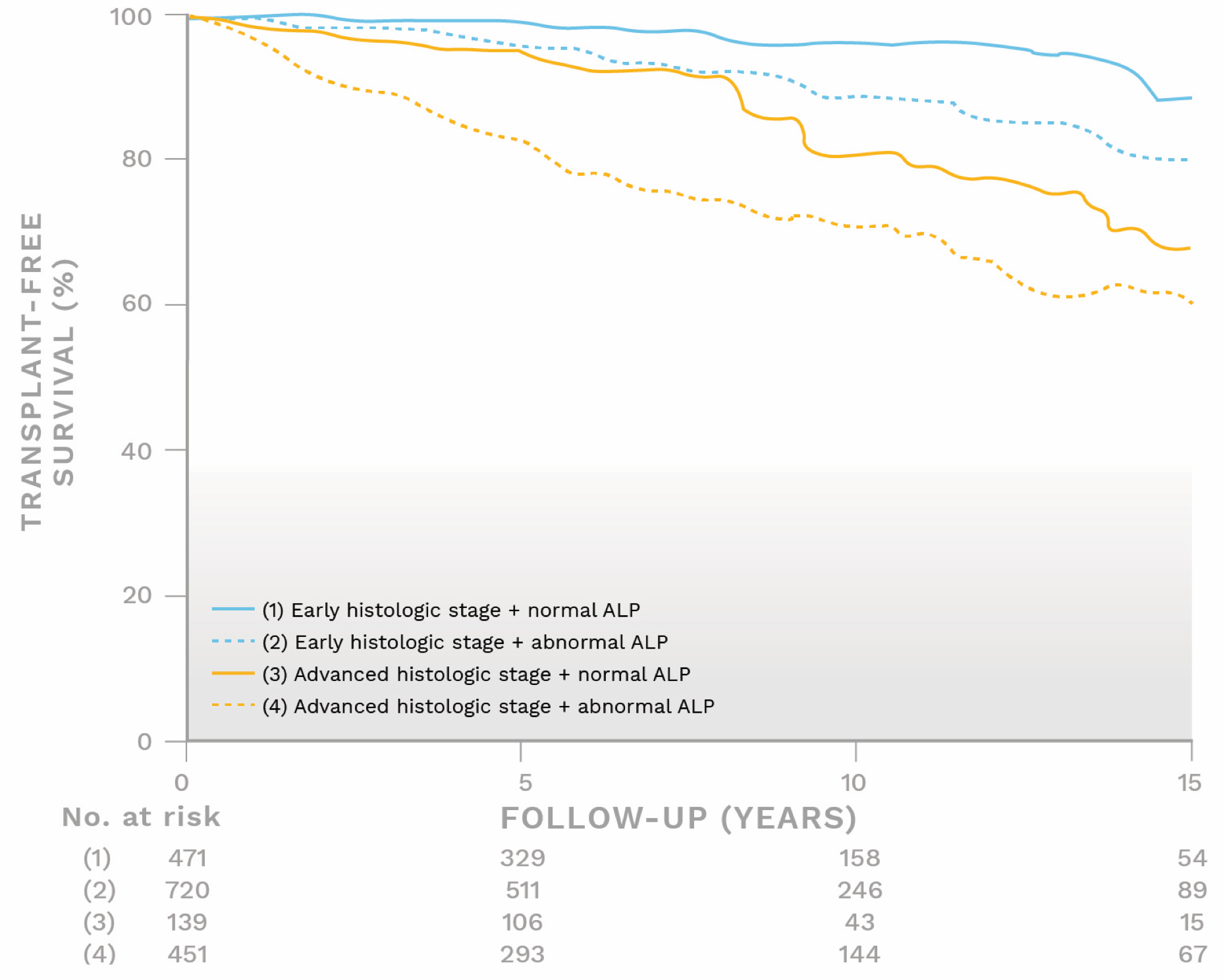
- Adapted from Murillo Perez CF, Hirschfield GM, Corpechot C, et al. Aliment Pharmacol Ther. 2019;50(10):1127-1136.
Patients with abnormal ALP and early fibrosis stage had similar transplant-free survival rates to those with normal ALP and advanced fibrosis stage (P=.12)
- Adapted from Murillo Perez CF, Hirschfield GM, Corpechot C, et al. Aliment Pharmacol Ther. 2019;50(10):1127-1136.
- a The Global PBC Study Group conducted an analysis including UDCA-treated and untreated patients diagnosed with PBC (N=3,059) with bilirubin levels ≤1x ULN at baseline or 1 year. The study explored optimal thresholds of bilirubin and ALP to predict liver transplantation or death. The association of ALP with survival was assessed in a subgroup of UDCA-treated patients with ALP ≤1.67x ULN and normal bilirubin at 1 year.1
- b Survival was defined as an absence of liver transplant and all-cause mortality.1
- c P value ≤.001 refers to the significant difference in survival rates for (1) ALP ≤1x ULN compared to (2) ALP 1x-1.67x ULN and (3) ALP 1.67x-3x ULN.1
- d The Global PBC Study Group conducted an analysis including UDCA-treated and untreated patients diagnosed with PBC (N=3,059) with bilirubin levels ≤1x ULN at baseline or 1 year. The study explored optimal thresholds of bilirubin and ALP to predict liver transplantation or death.1
- e P value <.001 refers to the significant difference in 10-year survival rates for the following: (1) bilirubin ≤0.6x ULN; (2) bilirubin >0.6x ULN; and (3) abnormal bilirubin.1
- f Calculation based on percent rates of liver transplant or death extrapolated from survival estimate curve at 10 years.1,2
- g Patients with abnormal bilirubin (≥1.2 mg/dL) were excluded from this analysis.1
- h P value <.001 refers to the significant difference in survival rates for (1) bilirubin 0.6x-1x ULN + ALP ≤1x ULN compared to (2) bilirubin 0.6x-1x ULN + ALP 1x-1.67x ULN and (3) bilirubin 0.6x-1x ULN + ALP >1.67x ULN. P values are a reflection of differences of the total curves.1,2
- i Data from the Global PBC Study Group were used, and this analysis included UDCA‐treated patients in whom a liver biopsy was performed at study entry in order to evaluate the utility of baseline fibrosis stage in predicting long-term outcomes in the context of biochemical risk stratification. Biopsies conducted in the 24 months prior to study entry and up to 12 months after study entry were considered baseline.3
- j Biochemical treatment response after 1 year of UDCA therapy was defined by Toronto and Paris II criteria.3
- k After 1 year of UDCA treatment.3
- ALP, alkaline phosphatase; PBC, primary biliary cholangitis; UDCA, ursodeoxycholic acid; ULN, upper limit of normal.
References:
1. Murillo Perez CF, Harms MH, Lindor KD, et al; the GLOBAL PBC Study Group. Goals of treatment for improved survival in primary biliary cholangitis: treatment target should be bilirubin within the normal range and normalization of alkaline phosphatase. Am J Gastroenterol. 2020;115(7):1066-1074. 2. Data on file: Intercept Pharmaceuticals, Inc. 3. Murillo Perez CF, Hirschfield GM, Corpechot C, et al; the GLOBAL PBC Study Group. Fibrosis stage is an independent predictor of outcome in primary biliary cholangitis despite biochemical treatment response. Aliment Pharmacol Ther. 2019;50(10):1127-1136.